A 35 year old man with complaints of Pain abdomen and fever since 5 days
A 35 year old man Artist by occupation from Choutuppal came to our hospital with
C/o Pain abdomen since 5 days and fever since 3 days
History of presenting illness
Patient was apparently asymptomatic 15 days ago.
He attended a party where he drank heavily and had heavy food, following morning patient developed Pain abdomen in the right hypochondriac region and epigastric region which was insidious in onset and gradually progressive and was associated with fever so he took some medication which subsided pain and fever for few hours. Pain was sudden, pricking type and was radiating to the back. Due to pain he stopped working.
Couple of days later he visited a hospital at Choutuppal as the pain was increasing where he was told to have Jaundice, Blood and urinary tract infection and was prescribed medication.
Patient had burning micturition and passed red colored urine for 3 days followed by yellow colored urine for about 5 days
Patient passed dark colored stools for 3-4 days.
1 week back he lost his appetite and was only having grapes and also couldn't sleep due to pain
5 days back Pain was severe which was again associated with fever so he came to our hospital.
No aggravating and relieving factors for pain
No h/o vomiting, chills and rigors, nausea, cough, body pains, diarrhoea.
Past history
No similar complaints in the past
Not a known case of Diabetes mellitus, Hypertension, Asthma, Epilepsy, Tuberculosis,CAD.
History of operation for Inguinal hernia 10 years back and met with an accident 8 years back for which he got stitches on his scalp
He is unmarried and stays alone by himself as his Father passed away in 2010 due to chronic alcoholism and his mother passed away in 2016 due to breast cancer during this time he got addicted to alcohol and cigarette smoking.
Personal history
Mixed diet
Appetite reduced since 1 week and patient only had grapes every day
Sleep inadequate since 1 week
Bladder movements regular
Constipated since 5 days as he is not having food
Addicted to alcohol and cigarette smoking since 10 years and smokes 20 cigarettes per day and drinks half bottle alcohol every day
During mornings he experiences tremors while painting which subsides after drinking 90ml of alcohol and also has a habit of continuous smoking during the day while working.
He stopped smoking 20 days back due to some restrictions in his work place
He stoped drinking 15 days back when he started experiencing pain abdomen following heavy drinking.
No history of drug addiction.
No allergies
He doesn't drink or smoke or eat Non-vegetaerian food for a fixed span of 50 days every year because of religious commitment and 10 days following that he has decreased cravings for alcohol and smoking.
Family history
No significant history
Tolerance present
Tremors present whenever he doesn't consume alcohol
Cravings for alcohol and tobacco present
Psychiatric history
No h/o head injury, seizures
No h/o low mood, suicidal thoughts
No h/o hearing of voices
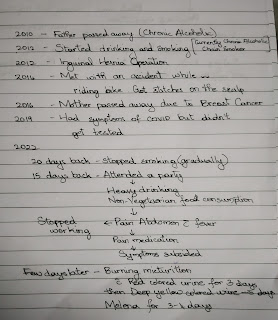
Time line
General examination
Concious, Coherent, Cooperative
Well oriented to time, place and person
BP-140/90 mm of Hg
Pulse rate - 90 bpm
Respiratory rate -20 cycles per min
Temperature - 102° F
SpO2- 92%
Pain - intermittent,Pricking type of pain in Right hypochondriac and epigastric region with no aggravating and relieving factor
Icterus present
No Pallor, Cyanosis, clubbing, Lymphadenopathy, Edema.
Systemic examination
CVS - S1, S2 heard, No murmurs
RS - NVBS +
Abdomen - Tenderness present in Right hypochondriac and epigastric region
No palpable masses
No free fluid in the abdomen
Liver not palpable
Spleen not palpable
Bowel sounds- sluggish
CNS - No focal neurological deficits
Provisional diagnosis
Liver abscess
Investigations
CBP
Hb- 12.2 mg/dL
TLC- 18,500
Platelets - 4.5 lacs
Serology - Seronegative for HCV, HBsAg, HIV 1 and 2
LFT
TB-5. 42
DB-3. 86
AST-163
ALT-139
ALP-603
TP-5. 3
A/b- 2.6
USG -shows 50% liquefaction
Abdomen PA/AP
Treatment
NS and RL
Inj. Metogryl
Inj. Pantop
Inj. Piftaz
Inj. Tramadol
Magnex
Thiamine
Inj. Diclofenac








Comments
Post a Comment